News & Events
News
The Gasette - Anesthesia Newsletter : February 2024
Here are the stories from the latest Anesthesia Newsletter:
- Testing the Feasibility of Anesthetic Methods in Microgravity
- Practice Ready Assessments as a Pathway to Licensure
- Improving Patient Access to Surgery
- Anesthesia Research Accountability Program
Read the newsletter here
Dal Anesthesiologists Test Feasibility of Anesthetic Methods for Use in Microgravity
Synopsis
With increasing space-based industry and exploration, the chances of serious injury continue to increase. A broken arm would not only mean suffering for an untreated astronaut, but could also compromise the mission and safety of other team members. Given the need to don a space suit and enter a small capsule for return to earth, extracting an injured astronaut would be incredibly difficult without pain medication. Technical and physiological challenges associated with the administration of general anesthesia in outer space make this not feasible. Other pain medications could compromise cognition and even decrease drive to breath, which could mean death during earth atmosphere re-entry. Dr. Jon Bailey, a Nova Scotia Health regional anesthesia specialist and assistant professor at Dalhousie University, has led a team to evaluate the feasibility of effectively using ultrasound-guided perineural injections to administer regional anesthesia, a technique used to numb a specific part of the body, in a simulated microgravity environment.
Background
In 1961, humanity made its historic first trip into space. Over the past six decades, the aerospace industry has flourished significantly, enabling crewed space missions such as moon landings and Mars exploration. Space agencies across the world are spending a significant amount of money and time to train astronauts for space missions. Essentially, everyone involved in these missions will run the risk of suffering serious injuries like burns and fractures. Injured astronauts in low-earth orbit could be returned to earth to receive treatment. However, a significant injury such as a broken arm could seriously interfere with an astronaut being able to don an extravehicular mobility unit (or ‘space suit’) or to be loaded into a cramped capsule for re-entry. If emergency extraction is not possible, as may be the case during trips to Mars, space surgery will be necessary to provide medical care and intervention until the personnel can return to Earth.
Overcoming the Challenges

The team (from left to right): Drs. Matthew Mackin, Mathew Kiberd, Jon Bailey, Regan Brownbridge (Not in photo): Drs. Sally Bird, Dan Werry, and Garrett Barry
Treating injuries in space comes with many challenges, including altered physiology, upper airway edema, and a very poor intubation rate in experiment models. Regional anesthesia has been suggested as a solution for providing analgesia and anesthesia in a microgravity environment, but the feasibility of performing blocks in microgravity has yet to be tested. Although the first anesthetic-assisted surgery on rodents occurred in 1990, no human has ever undergone surgery in space. As government space agencies and private companies have made significant plans for crewed spaceflights in the coming years, serious injuries are inevitable. As such, careful planning for pain management during extraction and even anesthesia for surgical procedures in microgravity is essential.
Dr. Jon Bailey, a Nova Scotia Health regional anesthesia specialist and an assistant professor in the Department of Anesthesia, Pain Management and Perioperative Medicine at Dalhousie University, has led a project to determine the viability of performing regional anesthesia in a simulated microgravity environment – underwater, to provide supporting evidence and data for administering regional anesthesia to space surgery patients. The Canadian Space Agency has utilized deep water for space exploration simulations, but no studies have been conducted in this setting to evaluate regional anesthesia.
To execute this project, Dr. Bailey put together a group of his anesthesiologist colleagues several of whom are also certified scuba divers to carry out this project. Team members include Drs. Mathew Kiberd, Regan Brownbridge, Garrett Barry, Matthew Mackin, Dan Werry, and Sally Bird. “The team came together fairly organically after I contacted the individuals who I thought would be a good fit. This is also a rare instance of a project where the majority of the people I spoke with were genuinely enthusiastic and wanted to participate.”
Findings

One of the meat models, encased with ballistic gel to avoid contact and to improve durability.
The team conducted two studies. In the first study, the team evaluated dye's discriminative ability in meat models, using beef tendon simulating nerves. 30 meat models were injected and scored for the ease of interpretation and accuracy. In the second study, the team used 40 meat models to evaluate the administration of regional anesthesia in two conditions: microgravity analogue and normal earth gravity. The models were secured to a mannikin and injected with dye in a perineural position using ultrasound guidance. The models were then stored in a refrigerator for 24 hours before being dissected and scored by two blinded assessors to evaluate success rate. The time required to perform the injection, ultrasound image quality, and needle placement ease in the microgravity analogue and normal earth gravity environment were also measured.
In the first study, the team found that the discriminative ability of the meat model was high. Blinded assessors correctly identified the position of the injected dye 100% of the time for injections correctly placed beside the ‘nerve’, 95% for injections inside the nerve, and 85% for injections inside the muscle. Overall agreement between assessors was 87% with a sensitivity of 100% and specificity of 90%. Determining the location of injection was deemed to be easy or very easy in 72% of the models.
The second study found that simple nerve blocks are feasible in a microgravity environment. The time to complete injection, ease of image acquisition, and number of accurately placed injections was not different between the groups. However, the team found that needle placement in a free-floating microgravity environment was more difficult than compared to a seated normal gravity condition.
 Performing dye injection on meat model with the use of ultrasound guidance.
Performing dye injection on meat model with the use of ultrasound guidance.
This project is a preliminary work that could pave the way for medical technique development that will ensure the safety of astronauts and the success of space missions. “Nerve blocks are very likely the safest way to provide pain control for an astronaut with an injury,” says Dr. Bailey. “The techniques to maximize effectiveness and safety haven’t yet been developed in microgravity.”
Research & Innovation
Dr. Bailey’s motivation to undertake research projects stems from his enthusiasm for novel ideas and unexplored areas. "Once I start, I feel compelled to see them through,” says Dr. Bailey. “None of this would be possible without incredible collaborators and mentors who break down barriers and keep the momentum going."
The project is the inaugural winning project of the Orlando Hung Innovation Fund (OHIF) Award. It is one of the Department's newest funding programs, as part of the Anesthesia Research Fund Awards. “It’s a huge honour to receive the inaugural Orlando Hung Innovation Fund grant,” says Dr. Bailey. The OHIF, named after Dr. Orlando Hung, is dedicated to supporting early ideas that can develop best practice models and procedures. Its goal is to facilitate systemic change and remove barriers that may hinder the timely development, assessment, and implementation of medical innovations that improve patient lives. “Dr. Hung has been an inspiring clinician, researcher, and humanitarian. I’m very grateful that our department has such strong support for research and innovation. This has allowed us to have an outsized impact nationally.”
"Having the award named after me is a tremendous honour, and I am truly grateful. It is my hope that this award will be able to contribute to the development of early studies of clinical, educational, research, or administrative innovations with the aspiration of ‘how we can always do better’”, says Dr. Orlando Hung. "I would like to congratulate Dr. Bailey and his team for this award to support their exciting project. I wish I could participate in their microgravity study because I missed the opportunity to conduct an Airway Management in microgravity study some years ago.”
Future Development
Dr. Bailey intends to engage in a collaborative effort with the Health Beyond Initiative of the Canadian Space Agency in order to advance and expand the research on the administration of regional anesthesia in microgravity settings. He also plans to carry out additional investigation by utilizing the model established in this project, such as instructing personnel without anesthesia expertise to execute the administration of blocks anesthesia, which could potentially yield practical implications for delivering healthcare in remote and extreme locations, such as during military and rescue operations. Additionally, one of the future goals pertains to the logistical aspects of creating a regional anesthesia kit specifically designed for utilization on the International Space Station.
The Gasette - Anesthesia Newsletter : November 2023
The November 2023 issue of our department's newsletter, which highlights our members' achievements in patient care, education, and research, is now available.
Read the newsletter here.
Dr. Orlando Hung – DMAA Exceptional Service Award
 Dr. Orlando Hung, staff anesthesiologist and former long-serving Medical Director of Research, was recently honoured for his legacy of exceptional work by being bestowed the Dalhousie Medical Alumni Association Exceptional Service Award. The award is presented annually to recognize alumni who are highly respected, and whose careers and service in the practice of medicine have been outstanding. Dr. Hung was nominated by Dr. André Bernard, for his significant impact on anesthesiology research, advanced airway management, and his compassionate character.
Dr. Orlando Hung, staff anesthesiologist and former long-serving Medical Director of Research, was recently honoured for his legacy of exceptional work by being bestowed the Dalhousie Medical Alumni Association Exceptional Service Award. The award is presented annually to recognize alumni who are highly respected, and whose careers and service in the practice of medicine have been outstanding. Dr. Hung was nominated by Dr. André Bernard, for his significant impact on anesthesiology research, advanced airway management, and his compassionate character.
“As a renowned academic physician with appointments in four departments and numerous publications, Dr. Hung has not only received all teaching awards within the Department, but also received recognition from the Canadian Anesthesiologists' Society,” says Dr. Bernard. “He has been a steadfast advocate for, and mentor and friend to medical students, supporting self-led initiatives, philanthropy, and student fundraising.”
Dr. Hung has fostered local and international development through his genuine interest in the well-being of others and his sense of hospitality. As a volunteer with the Canadian Anesthesiologists’ Society International Education Foundation, he has contributed over 1000 hours to the development of the residency program at the National University of Rwanda, demonstrating his humanitarian efforts to improve safe anesthesia globally.
“I am incredibly honoured to receive this prestigious award,” says Dr. Hung. “The processes of teaching, learning, and providing healthcare are ongoing endeavors that have no end in sight. I am always broadening my horizons in order to support my fellow colleagues and learners, and to provide excellent care to our patients.”
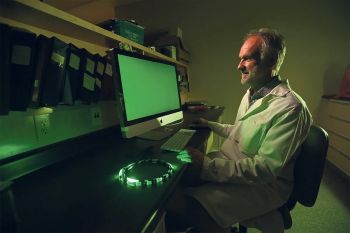
Dr. Jason McDougall is exploring the potential of using green light therapy to alleviate osteoarthritis pain
Green light for osteoarthritis pain relief
 Pain is often invisible – but its impact can be devastating. Almost two-thirds of people living with osteoarthritis report they don’t experience adequate pain relief.
Pain is often invisible – but its impact can be devastating. Almost two-thirds of people living with osteoarthritis report they don’t experience adequate pain relief.
“People are sometimes told to ‘just get on with it.’ Personally, I find this unacceptable,” says Dr. Jason McDougall, a pain management researcher at Dalhousie University.
With funding support from Arthritis Society Canada, Dr. McDougall is now investigating the potential of green light therapy as a “cheap, safe, non-invasive and easy-to-use” approach to arthritis pain management.
“Viewing a specific green light for one to two hours a day has been found to be effective for conditions like migraine and fibromyalgia, so we are going to test it with osteoarthritis pain,” he says.
Results from preclinical trials conducted on animal models have been promising – showing “dramatically reduced pain levels – even beyond what we would see with classic drug treatments,” says Dr. McDougall, who is especially interested in better understanding the precise mechanism whereby the green light perceived by the retina then affects the brain regions involved in managing pain. The next step is a small clinical trial for people with osteoarthritis.
Beyond helping patients for whom traditional pharmacological approaches haven’t been effective, Dr. McDougall says green light therapy could be used as an additional treatment to reduce reliance on non-steroidal anti-inflammatory pain medications or opioids.
He is also excited about evidence showing that green light therapy might improve an individual’s mood. Canadians with arthritis are nearly twice as likely to have a mood disorder like depression compared to those without arthritis.
“This research is innovative, and the rewards could be revolutionary,” adds Dr. McDougall.
This article originally appeared in a Globe and Mail sponsor content feature produced by RandallAnthony Communications.
Reprinted with permission. All rights reserved.
